Legacy media finally catches up: Covid patients are oxygen-starved and do poorly on ventilators
By TATIANA PROPHET
Doctors at Providence Hospital in Seattle observed that the very first known U.S. patient to have Covid-19 was suffering from a lack of oxygen. That was back in January 2020.
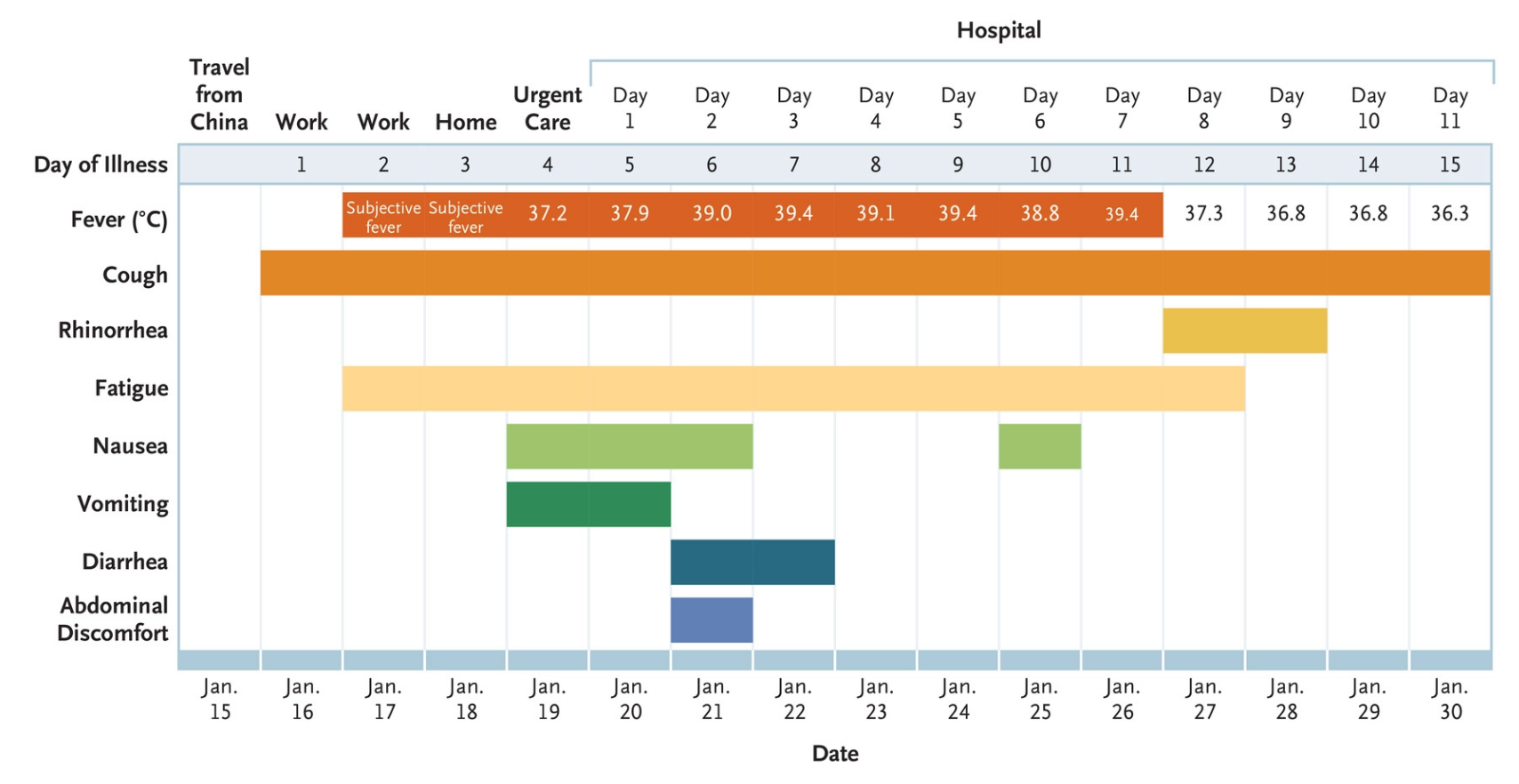
The unnamed patient, who reported to urgent care after four days of fever and a dry cough, was tested due to having just returned from Wuhan, China. After testing positive for 2019-nCoV, he was hospitalized on January 21 in an isolation room.
At first, his blood-oxygen saturation levels were within the normal 96%-98% range, and he did not have shortness of breath, but did have a cough and two days of nausea and vomiting, according to the New England Journal of Medicine. A chest x-ray on day 3 showed no abnormalities.
Patient zero was never put on a ventilator; instead, his doctors noted growing evidence of pneumonia coupled with low blood-oxygen saturation rates. He received supplemental oxygen, two kinds of antibiotics for a possible hospital-derived infection — and experimental drug Remdesivir for compassionate use.
The very next day, he began improving. On day 8, oxygen levels showed normal “and the previous bilateral lower-lobe rales were no longer present” in the lungs..
March 26: UK-based Express warned readers that blue lips may be a sign of an emergency that requires dialing “999.”
April 8: Dr. Dave Clark posted on the web site for the Coalition for Hemophilia B that he was hearing that doctors in China, Italy and New York, noticed that something beyond pneumonia was going on and that hypoxia might be the culprit.
“The lungs are marvelously complex ‘machines’ that transfer oxygen from the air we breathe into red blood cells (RBCs) that can then move that oxygen throughout the body to the tissues that need it. At the same time, the RBCs move carbon dioxide (CO2), which is a waste product, from the tissues back to the lungs where it is exhaled. When something goes wrong and the body is not getting enough oxygen, we tend to first suspect the lungs. For one thing, because the lungs behave like machines, we can more easily understand how they work. The rest of the process of moving oxygen and CO2 is all chemistry, so takes more effort to tease out what’s actually going on.”
April 8: Stat News, the Boston Globe’s health news service, published an article quoting physicians saying that ventilators may be the wrong tool for Covid-19 patients, many of whom are starving for oxygen in their blood. “some critical care physicians are questioning the widespread use of the breathing machines for Covid-19 patients, saying that large numbers of patients could instead be treated with less intensive respiratory support. If the iconoclasts are right, putting coronavirus patients on ventilators could be of little benefit to many and even harmful to some.”
April 16: Danielle DiCenso, a 33-year-old nurse at Palmetto General Hospital, died at home after getting Covid-19 symptoms. That night, she told her husband she felt all right.
" It looked like the oxygen was just taken out of her," he told CBS12 News.
‘Happy hypoxia:’ May 7, CNN published an article about a particular characteristic of some Covid-19 patients, where they feel like everything is fine, and even when hospitalized are checking social media and chatting with nurses, while their blood-oxygen saturation levels are dangerously low.
New Hampshire ER Dr. Richard Levitan, who spent nearly two weeks volunteering in New York City, according to CNN said he “watched patients come into the emergency room with blood oxygen levels as low as 50%, so low they should have been incoherent, even unconscious. Normal blood oxygen saturation is between 95% and 100%, and anything below 90% is considered abnormal. In addition, Levitan said, scans of these patients' lungs showed signs of pneumonia so severe they should be in terrible pain as they gasp for their next breath.”
May 8: National Geographic published an article about the strange hypoxia occurring in Covid-19 patients. “Silent hypoxia has surprised many doctors,” wrote Maya Wei-Haas. “Some patients are running so low on oxygen, health-care workers would normally expect them to be incoherent or in shock. Instead, they’re awake, calm, and responsive. They chat with the physicians. They use their cell phones. While the basic physiology behind why these patients don’t immediately feel short of breath is well understood, scientists are still trying to come to grips with exactly how COVID-19 ravages the body, and why this disease, in particular, can quietly take your breath away.”
May 11: The Wall Street Journal published an article entitled “Some Doctors Pull Back on Using Ventilators to Treat Covid-19 Physicians report numbers of patients who are able to tolerate very low blood-oxygen levels,” and in the first sentence they say “large numbers” of patients are experiencing hypoxia.
“People with Covid-19 began showing up at the hospital with rarely seen, ultra-low blood-oxygen levels. Even for those who weren’t struggling to breathe, doctors were concerned that patients’ conditions could suddenly worsen, which with Covid-19 could swiftly turn deadly. So they often intubated sooner. “In the past, you’d see these kinds of oxygen levels, and your brain would intuit all these other things,” said Scott Weingart, chief of emergency critical care in the department of emergency medicine at Stony Brook Hospital in Stony Brook, N.Y. “For instance, you’d assume the patient’s lungs must be so bad that if we don’t intubate now, they might crap out.”
Many of us who follow the testimonials coming from ICU and ER staff about coronavirus already knew about the sudden hypoxia that can take over and make patients critical in the blink of an eye. That’s because on April 1, Brooklyn ER doctor Cameron-Kyle Sidell made a YouTube video in his kitchen stating that ventilators were the wrong tool for many of the Covid patients he saw. Their lungs were working fine; it was the levels of oxygen in their blood that were extremely low, also known as hypoxia.
Explained Dr. Dave Clark on the Hemophilia B web site: “Hemoglobin is the molecule inside your red blood cells (RBCs) that carries oxygen. The RBCs pick up oxygen in the lungs and carry it around the body, releasing it to the cells and tissues that need it. The normal oxygen range for a health patient is 95–100%, which means that 95–100% of the hemoglobin in your blood has oxygen bound to it. Below about 89%, the body starts to have trouble from a lack of oxygen.”
“Some research has shown that a number of the proteins generated by the novel coronavirus can bind to hemoglobin. Those proteins might be throwing off the oxygen test and interfering with the red blood cells’ ability to carry oxygen. This is where the drugs hydroxychloroquine (HCQ) and chloroquine (CQ) might come in. These drugs are derivatives of quinine, which was the original treatment for malaria. The malaria parasite (not a virus) has developed resistance to all three of these drugs, so in many parts of the world these drugs are not used very much for treating malaria. However, HCQ has found uses in treating lupus and rheumatoid arthritis. We still don’t fully know how these drugs work, but there is some speculation that they stabilize hemoglobin, among other things. The malaria parasite feeds on hemoglobin. One idea is that HCQ stabilizes the hemoglobin and starves the parasite.”
The recent observational study about hydroxychloroquine stating that it made no difference involved extremely critical patients; back on March 20 when French virologist Didier Raoult published results of his use of hydroxychloroquine, he said dosage was crucial. He also said use of antibiotics to take care of opportunistic bacteria, plus zinc, was important.
Legacy media has caught up to the lack of oxygen; will they finally catch up to the hemoglobin-malaria connection, and thus the (judicious) use of hydroxychloroquine? How many lives have to be lost before they do?